[under construction]
I'm always stunned at how the interests of large argi-business and politicians seem to go hand in hand.
Our "food-makers" do anything, moral and [mostly] immoral, they can to make more money and the government says "it's okay with me" and taxes us for everything the agri-businesses put into our supermarkets.
We end up having little choice but to eat and get sick.
Look at your supermarket.
It's full of non-food.
Chemicals, pesticides, irradiation, additives, emulcifiers.
e.g. you don't trust civic water,
so you buy water in plastic bottles
which have chemicals that mimic estrogen,
so guys get man-tits
Who/what does this benefit?
Certainly not our intestinal systems.
here's a few stories from alternet to help you think this over.
1 how to stop encouraging corporate argi-business
2 Parkinson's and pesticides
3 Bisphenol A and heart disease in women
[my comments- Costick67]
1

[pic: "will work for food; non-GM food, that is."]
Joel salatin on defeating corporate food
Excerpted by permission from "Declare Your Independence" by Joel Salatin, part of the book Food, Inc., available now from PublicAffairs. Copyright 2009.
Perhaps the most empowering concept in any paradigm-challenging movement is simply opting out. The opt-out strategy can humble the mightiest forces because it declares to one and all,
"You do not control me."
[This is the gist of all my arguments. YOU choose to change. You don't need your oppressors' permission. That would land you in jail.]
The time has come for people who are ready to challenge the paradigm of factory-produced food and to return to a more natural, wholesome and sustainable way of eating (and living) to make that declaration to the powers that be, in business and government, that established the existing system and continue to prop it up. It's time to opt out and simply start eating better -- right here, right now.
Impractical? Idealistic? Utopian? Not really. As I'll explain, it's actually the most realistic and effective approach to transforming a system that is slowly but surely killing us.
What happened to food?
First, why am I taking a position that many well-intentioned people might consider alarmist or extreme? Let me explain.
At the risk of stating the obvious, the unprecedented variety of bar-coded packages in today's supermarket really does not mean that our generation enjoys better food options than our predecessors. These packages, by and large, having passed through the food-inspection fraternity, the industrial food fraternity and the lethargic cheap-food-purchasing consumer fraternity, represent an incredibly narrow choice.
If you took away everything with an ingredient foreign to our 3 trillion intestinal microflora, the shelves would be bare indeed. (I'm talking here about the incredible variety of microorganisms that live in our digestive tracts and perform an array of useful functions, including training our immune systems and producing vitamins K and biotin.) In fact, if you just eliminated every product that would have been unavailable in 1900, almost everything would be gone, including staples that had been chemically fertilized, sprayed with pesticides or ripened with gas.
Rather than representing newfound abundance, these packages wending their way to store shelves after spending a month in the belly of Chinese merchant marine vessels are actually the meager offerings of a tyrannical food system.
Strong words? Try buying real milk -- as in raw. See if you can find meat processed in the clean open air under sterilizing sunshine. Look for pot pies made with local produce and meat. How about good old unpasteurized apple cider? Fresh cheese? Unpasteurized almonds? All these staples that our great-grandparents relished and grew healthy on have been banished from today's supermarkets.
They've been replaced by an array of pseudo-foods that did not exist a mere century ago. The food additives, preservatives, colorings, emulsifiers, corn syrups and unpronounceable ingredients [crimes, all crimes.] listed on the colorful packages bespeak a centralized control mind-set that actually reduces the options available to fill Americans' dinner plates.
Whether by intentional design or benign ignorance, the result has been the same -- the criminalization and/or demonization of heritage foods. The mind-set behind this radical transformation of American eating habits expresses itself in at least a couple of ways.
One is the completely absurd argument that without industrial food, the world would starve. "How can you feed the world?" is the most common question people ask me when they tour Polyface Farm.
Actually, when you consider the fact that millions of people, including many vast cities, were fed and sustained using traditional farming methods until just a few decades ago, the answer is obvious. America has traded 75 million buffalo, which required no tillage, petroleum or chemicals, for a mere 42 million head of cattle. Even with all the current chemical inputs, our production is a shadow of what it was 500 years ago. Clearly, if we returned to herbivorous principles five centuries old, we could double our meat supply. The potential for similar increases exists for other food items.
The second argument is about food safety. "How can we be sure that food produced on local farms without centralized inspection and processing is really safe to eat?"
Here, too, the facts are opposite to what many people assume. The notion that indigenous food is unsafe simply has no scientific backing. Milk-borne pathogens, for example, became a significant health problem only during a narrow time period between 1900 and 1930, before refrigeration but after unprecedented urban expansion. Breweries needed to be located near metropolitan centers, and adjacent dairies fed herbivore-unfriendly brewery waste to cows.[Crimes, all crimes.] The combination created real problems that do not exist in grass-based dairies practicing good sanitation under refrigeration conditions.
Lest you think the pressure to maintain the industrialized food system is all really about food safety, consider that all the natural-food items I listed above can be given away, and the donors are considered pillars of community benevolence. But as soon as money changes hands, all these wonderful choices become "hazardous substances," guaranteed to send our neighbors to the hospital with food poisoning.
Maybe it's not human health but corporate profits that are really being protected.
2
Robin marantz herig
parkinsons from pesticides?
This story originally appeared in OnEarth Magazine.
Jackie Christensen was 32 when her body began to betray her. She had just returned to work after the birth of her second son and when she tried to type, two fingers on her left hand refused to cooperate. "They wouldn't go where I would want them to on the keyboard," says Christensen, who at the time -- it was 1997 -- was co-director of the food and health program at the Institute for Agriculture and Trade Policy, a Minneapolis think tank. "I also had what they frequently call frozen shoulder, with a very low range of motion in my left arm."
The first neurologist Christensen went to responded flippantly to her suggestion that she might have multiple sclerosis, which she had self-diagnosed because of her relatively young age and the fact that she was female. "If you want me to write that down, I will," she remembers him saying, refusing to pursue the matter further. A second neurologist thought it was all in Christensen's mind and referred her to a psychiatrist. Over the next several months, her symptoms got progressively worse, and she finally consulted neurologist number three. His startling diagnosis: Parkinson's disease.
"I thought, 'I can't have Parkinson's because I'm not old,'" Christensen recalls. But a trial of the standard treatment, a drug called L-dopa, seemed to work. Based on that clinical observation, the diagnosis was confirmed. This was in 1998, when Christensen was not quite 35, and she has been on L-dopa, with varying degrees of success, ever since.
Why did a disease that usually affects people in their sixties and seventies, and that affects men more often than women, strike this vibrant young mother? Christensen, a lifelong environmental activist, suspected an environmental cause -- not only because she was politically inclined to, but because she knew that accumulating scientific information was pointing in that direction. In the past few years, Christensen has been part of a movement exploring a possible connection between exposure to environmental toxins -- in particular, the organophosphate pesticides -- and Parkinson's disease, through her work with the Collaborative on Health and the Environment, a national network of advocacy and scientific organizations. She is co-founder of CHE's working group on Parkinson's Disease and the Environment.
A cause-and-effect relationship between environmental neurotoxins and Parkinson's is difficult to prove. As with many other scientific efforts to establish disease causation through population studies, there will probably never be a smoking gun that settles things once and for all. Population studies can detect associations between certain suspected agents and diseases such as cancer, but it's hard to draw conclusions about what causes a disease from studies that can register only correlations. In the case of Parkinson's and the environment, however, there has been a steadily mounting consensus about such a connection, and the pace has quickened in the past year or so.
A January 2009 consensus statement from CHE, in collaboration with the Parkinson's Action Network, a patient advocacy group, found that there was "limited suggestive evidence of an association" between pesticides and Parkinson's, and between farming or agricultural work and Parkinson's. This followed by just a few months the publication of Environmental Threats to Healthy Aging, a report co-authored by the Science and Environmental Health Network, a consortium of advocacy groups based in Ames, Iowa; it included a summary of 31 population studies that have looked at the possible connection between pesticide exposure and Parkinson's. Twenty-four of those studies, according to the report, found a positive association, and in 12 cases the association was statistically significant. In some studies, the group found, there was as much as a sevenfold greater risk of Parkinson's in people exposed to pesticides. In addition, in April 2009, scientists at the University of California, Los Angeles (UCLA), published a provocative study connecting the disease not only to occupational pesticide exposure but also to living in homes or going to schools that were close to a pesticide-treated field. ["I ain't gonna go to school!""I'll get me sick". How can you argue with that?]
Taken together, 30-plus years of research add up to an increasingly persuasive conclusion: exposure to pesticides and other toxins increases the risk of Parkinson's disease, and we are only now beginning to wrestle with the true scope of the damage.
Parkinson's is the second most common neurodegenerative disease (after Alzheimer's) in the United States, affecting between 1 million and 1.5 million Americans. The majority of cases occur in people over 65, about 60 percent of them male. It leads to uncontrollable tremors, muscle rigidity, and the inability to direct your arms or legs to move when you want them to. People with Parkinson's often have a masklike, impassive expression. They may have difficulty speaking clearly and develop a characteristic shuffling gait. Cognitive skills usually are not affected, though some functions like memory and decision-making can be impaired, and, in the face of the gradual and inevitable encroachment of physical limitations, people with Parkinson's often become depressed.
In part because it can take many forms, Parkinson's disease is difficult to diagnose. Several movement disorders have been classified in the general category known as Parkinson's-like syndrome, or parkinsonism. Scientists are divided about whether Parkinson's disease and parkinsonism are even related in any meaningful way, beyond sharing some symptoms. The two conditions may not even involve the same brain defects. The strict definition of Parkinson's disease is a loss of cells in the substantia nigra, a small structure in the basal ganglia region of the midbrain (though other brain structures are now thought to be involved as well). The substantia nigra ordinarily secretes the neurotransmitter dopamine,[the real dope] which is involved in many of the brain's functions, including the control of motor activity.
Often a diagnosis of Parkinson's disease is made the way it was made for Christensen: by a trial run of L-dopa, which boosts dopamine in the brain. If it works, the problem must be Parkinson's. It's a circular kind of logic, but it's all that most doctors have. There still are no definitive blood tests or brain scans to make the diagnosis.
In trying to establish risk factors for Parkinson's, one of the first decisions investigators must make is which cases to include in their epidemiological studies. Some studies include all patients, those with parkinsonian syndrome as well as those with definitively diagnosed Parkinson's. Some researchers limit their study subjects to people with Parkinson's disease and a demonstrated reduction of dopamine.
One of the more restrictive studies is a small subset of the massive Agricultural Health Study (AHS), which began in 1993 and involves nearly 90,000 individuals licensed to apply pesticides to crops, as well as their families. The AHS, conducted by the National Cancer Institute and the National Institute for Environmental Health Sciences with funding from the Environmental Protection Agency and the National Institute of Occupational Safety and Health, has tracked these workers to determine their risk of developing cancer and other serious diseases.
In 2002, scientists decided to look at a segment of this large database to assess the environmental risks for Parkinson's. This study-within-a-study, with the catchy acronym FAME (Farming and Movement Evaluation), compared the pesticide exposure of 114 AHS participants who have Parkinson's disease, as diagnosed by two specialists from the team, with exposure among 384 control cases matched for age, sex, and state of residence (either Iowa or North Carolina, where all the subjects are from). A group of scientists led by Caroline Tanner of the Parkinson's Institute of Sunnyvale, California, and Freya Kamel of the National Institute of Environmental Health Sciences looked at five possible risk factors in these 498 individuals: pesticide exposure; exposure to other neurotoxins; lifestyle factors such as diet, smoking, and caffeine use; the amount of melanin, or pigment, in the skin; and specific genetic variations, particularly those in genes involved in the production of dopamine or the metabolism of xenobiotics -- non-natural chemicals such as drugs and toxins that are transported and detoxified through pathways that scientists already understand.
The FAME study, the results of which are being prepared for publication next year, found that pesticide exposure was a significant risk factor for Parkinson's disease. The parent AHS study found that people who had been exposed to pesticides sporadically over a lifetime were 1.2 times more likely to develop Parkinson's than those who had not been. And when the exposure was heavy -- the kind of lifetime exposure seen in career pesticide applicators, or a single massive exposure as the result of a spill -- that increased risk jumped to 2.3 times. The riskiest pesticides were found to be some of those most commonly used in American agriculture, among them Paraquat and Trifluralin, both herbicides used to kill broadleaf weeds in food crops. (Paraquat is now restricted to commercially licensed users in the United States because of its toxicity, but it remains the second most widely used herbicide in the world, applied to more than 50 crops in 120 countries.)
These results were part of a cascade of findings pointing to a connection between environmental toxins, especially pesticides, and Parkinson's disease. As long ago as the 1970s, epidemiologists noticed that Parkinson's was more likely to occur in people who had grown up in rural areas, especially those who had lived on farms. But they were not sure which aspect of a rural background was relevant. Living near livestock? Drinking well water? Being exposed to pesticides? "It's been very difficult to pin down an explanation," Kamel says.
3
Elizabeth grossman
Bisphenol A
A study released this week by researchers at the University of Cincinnati says that exposure to bisphenol A may increase heart disease in women.
Bisphenol A (BPA) is the chemical building block of polycarbonate plastics and is used in countless consumer products including food and beverage containers, kitchen appliances, electronics, and packaging and is used to make resins that line food and drink cans.
Research by Scott Belcher and colleagues in the university's department of pharmacology and cell biophysics has found that environmentally available levels of BPA -- a synthetic chemical known to mimic the behavior of estrogen -- can disrupt normal heart muscle function and prompt arrhythmia or irregular heartbeat.
BPA has come under increasing scrutiny by medical researchers for its endocrine-hormone-disrupting potential -- effects that include interference with reproductive, egg and fat cell development, as well as with thyroid hormone and neurological functions. The chemical has also been linked to conditions that can prompt obesity and diabetes.
Additional cause for concern is the fact that these adverse effects can occur at very low levels of exposure.
"Levels of bisphenol A identified in human blood that would be in direct contact with the heart" can produce the effects seen in our research, said Belcher, speaking from Washington, where this research was presented at the June 10-13 Endocrine Society annual meeting.
While it creates plastics so durable they are used in sports gear, motor vehicles, shatterproof lenses as well as in baby bottles and toddlers sippy cups, the chemical can leach from finished products. These plastics and resins are so widely used that researchers studying the chemical describe BPA as ubiquitous. And although BPA does not last long in the environment or the human body, because it is so prevalent, current exposure in the U.S. is considered virtually continuous.
Monitoring by the U.S. Centers for Disease Control and Prevention (CDC) has found BPA in nearly 95 percent of the Americans tested. A recent study by Health Canada found BPA in 96 percent of the canned soft drinks it tested -- a study that covered 84 percent of all soft drinks sold in Canada -- at levels equivalent to 500 times what are considered normal estrogen levels.
Belcher's study showed that environmentally relevant, low levels of BPA can interfere with the genetic receptors that help regulate cardiac muscles, resulting in an increased frequency of irregular heartbeat. As an estrogenic compound, explains Belcher, the BPA interferes with how the heart muscle cells process calcium, a key factor in maintaining normal, healthy heartbeat. Due the specific ways in which the female body responds to estrogenic substances, this effect occurred in females rather than males.
One in three women in the U.S. suffer from cardiovascular disease, and women account for over 50 percent of the U.S. deaths from heart attack, so this finding could have wide ramifications.
According to the American Heart Association, women have a higher rate of death from a repeat -- rather than first -- heart attack, making any factors that could increase the risk of subsequent heart attack of particular concern.
Thus far, the adverse impacts of BPA on cardiac muscle cells have been seen in cells isolated from rat and mouse hearts. But Belcher says the genetic mechanisms affected should work the same way in the human heart. A statement on endocrine-disruption chemicals -- such as BPA -- just released by the Endocrine Society notes that the way these chemicals work is comparable in wildlife and in humans and in both live-animal and cell-culture experiments. Belcher's group is in the process of looking at cells isolated from human heart transplant samples.
Bisphenol A is currently approved by the U.S. Food and Drug Administration for use in food contact and other consumer products. But as evidence of the chemical's potential adverse health impacts grows, there are increasing efforts to regulate the compound.
Numerous states have introduced bills that would bar BPA from infant and children's products, but thus far only two have passed, one in Chicago, the other in Minnesota. However, a number of U.S. retailers have withdrawn such products voluntarily, among them Wal-Mart and Toys R Us. Canada has banned BPA from baby bottles sold there and now includes BPA on its list of toxic substances.
The chemical and plastics industry maintains that BPA is safe, as does the North American Metal Packaging Alliance, whose members use BPA in food-can lining. "The science supporting the safe use of epoxy liners in food contact applications is both extensive and extensively analyzed," said a statement released by NAMPA on May 30 in response to news media reports of a plastics and packaging industry meeting convened to craft a campaign to defend BPA safety.
"The scientific evidence supporting the safety of bisphenol A has been repeatedly and comprehensively examined by government and scientific bodies worldwide. In every case, these assessments support the conclusion that bisphenol A is not a risk to human health at the extremely low levels to which people might be exposed," says a statement from the Polycarbonate/BPA Global Group of the American Chemistry Council.
Responding specifically to Belcher's study and other as-yet-unpublished research presented at the Endocrine Society meeting, the ACC said, "Bypassing the scientific process in favor of sensational press releases is a scare tactic that will not promote public health." The ACC also questions the relevance to human health of BPA research conducted with animals.
"It should be noted that the Endocrine Society's conclusions directly conflict with the findings of authoritative scientific reviews," the ACC said in an additional statement released June 10. "In fact, the International Union of Pure and Applied Chemistry (IUPAC) has stated it is 'somewhat reassuring that after substantial research in the past decade, there have been no conclusive findings of low-level environmental exposures to EAS [endocrine active substances] causing human disease."
While not confirmation of any direct cause and effect, research published last year in the Journal of the American Medical Association found that people exposed to higher levels of BPA are more likely to develop cardiovascular disease than those who were not. This study was based on samples from nearly 1,500 adults collected by the CDC's National Health and Nutrition Examination Survey.
"For women, exposure to any environmental estrogens could be very important after a heart attack," said Belcher. Many women also experience arrhythmia during pregnancy, and the severity of an existing arrhythmia can worsen during pregnancy, so anything that would increase such risks would be of concern to both maternal and fetal health.
Given the strong evidence of multiple adverse health impacts of endocrine-disrupting chemicals such as bisphenol A, the Endocrine Society -- which has over 14,000 members from over 100 countries -- recommends decreasing exposure to these chemicals. Meanwhile, the FDA is continuing its own review of BPA safety.
---the end
-Costick67 ( 8^P
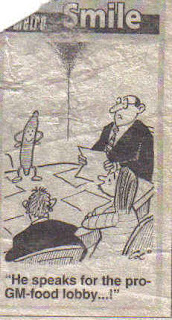
 [pic Pagliaccio]
[pic Pagliaccio]

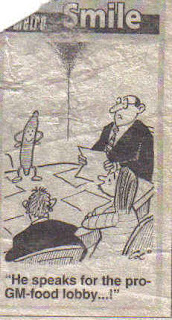





 (copyright, the Guardian 1999)
(copyright, the Guardian 1999)